Workup Health Guide
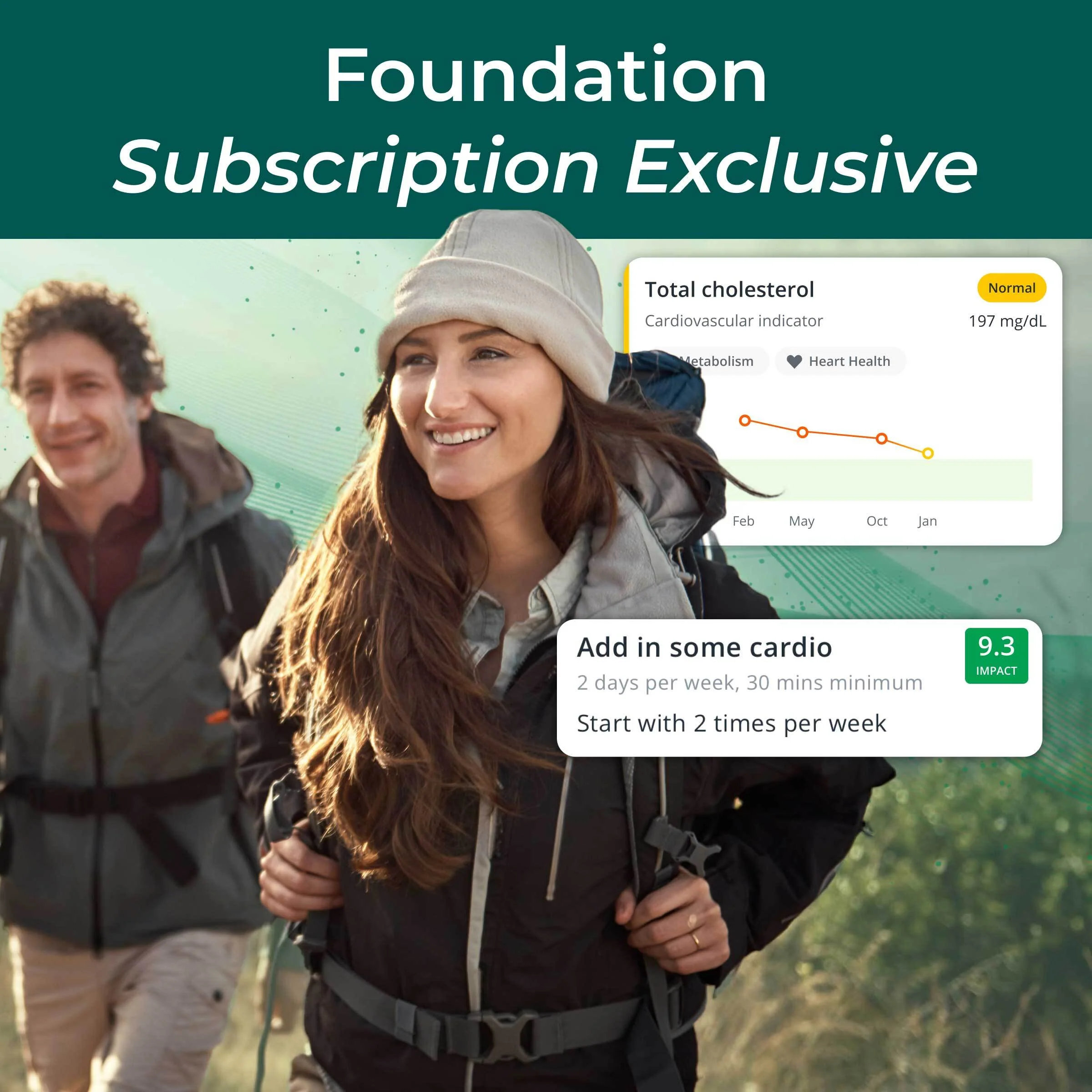
Personalized wellness insights powered by Workup’s AI — designed to help you explore health solutions aligned with your goals.
Profile Overview
Disclaimer: This report was produced using Workup’s AI recommendation engine, which evaluates your demographic and health information to identify potentially relevant products and services from vetted partners. Workup does not practice medicine, and this content is for informational purposes only. Consult your physician or licensed practitioner before making any healthcare decisions.
Overview
This guide is tailored for a 47-year-old male in Chicago, IL, focusing on managing hypertension to enhance cardiovascular health, longevity, and energy levels. It offers insights into preventive strategies that can make a significant impact on well-being.
Diagnostics & Screenings
For a 47-year-old man with hypertension aiming for cardiovascular health, longevity, and better energy, prioritize tight blood-pressure control, refine 10-year ASCVD risk, and detect early metabolic and kidney changes from hypertension. Pair foundational monitoring (home BP) with annual labs (lipids, A1C, kidney/liver), risk-refinement tools (hs-CRP, coronary calcium if decisions are uncertain), and age-appropriate cancer screening (colorectal). Screen for sleep apnea to improve BP and daytime energy. Increase test frequency if results are abnormal or medications change.
Screening Overview
| Tier | Test | Risk Area | Frequency | Why It Matters |
|---|---|---|---|---|
| Foundational | Home blood pressure monitoring | Uncontrolled hypertension and cardiovascular events | Check at home 2–3 days per week (two readings morning and evening); daily for 1–2 weeks after any medication change. | Nearly 1 in 2 U.S. adults has hypertension, and every 20 mmHg higher systolic or 10 mmHg higher diastolic BP roughly doubles risk of death from heart disease and stroke. Regular home monitoring improves BP control and reduces events. |
| Cardiovascular | Fasting lipid panel (total, LDL-C, HDL-C, triglycerides) | Atherosclerotic cardiovascular disease (ASCVD) | At least annually with hypertension; every 6–12 months if on statins or if results are borderline. | Heart disease is the leading cause of death. Lowering LDL-C by ~39 mg/dL (1 mmol/L) reduces major vascular events by about 20–25% in trials. |
| Cardiovascular – Advanced | Coronary artery calcium (CAC) scan (non-contrast CT) | Hidden coronary plaque burden to refine statin and aspirin decisions | One-time in the late 40s–50s to clarify risk; repeat in ~5 years if CAC=0 and risk factors change. | A CAC score of 0 predicts very low 10-year event risk (~1%); CAC ≥100 is linked to a 7–10× higher risk versus CAC=0. This helps target preventive therapies to those who benefit most. |
| Metabolic | Hemoglobin A1C | Diabetes and prediabetes (hypertension increases risk) | Every year; every 3–6 months if prediabetes or on glucose-lowering therapy. | About 1 in 10 U.S. adults has diabetes and over 1 in 3 has prediabetes; more than 1 in 5 people with diabetes are unaware. Early control prevents kidney, eye, nerve, and heart complications. |
| Organ Function – Kidney | Urine albumin-to-creatinine ratio (ACR) | Early hypertensive kidney disease and cardiovascular risk | Annually with hypertension; every 6 months if albuminuria is present or rising. | Chronic kidney disease affects ~15% of U.S. adults. Albuminuria can appear years before eGFR declines and independently predicts cardiovascular events. |
| Organ Function – Comprehensive | Comprehensive metabolic panel (CMP) with creatinine/eGFR and electrolytes | Medication safety and liver/kidney function with hypertension treatment | Every 6–12 months if taking ACE inhibitors, ARBs, or diuretics; at least annually otherwise. | Blood pressure medicines can change potassium and creatinine. Nonalcoholic fatty liver disease affects ~25% of adults and is often silent—routine labs detect issues early. |
| Inflammation | High-sensitivity C-reactive protein (hs-CRP) | Inflammatory cardiovascular risk not captured by LDL | Every 1–3 years to refine ASCVD risk and guide intensity of prevention. | hs-CRP ≥2 mg/L is associated with roughly 2× higher risk of heart attack and stroke independent of cholesterol levels. |
| Cancer | Colorectal cancer screening (FIT annually or colonoscopy every 10 years) | Colorectal cancer (age ≥45) | Start now at 47: do a yearly FIT stool test, or a colonoscopy every 10 years if results are normal. | Colorectal cancer is the 2nd leading cause of U.S. cancer death; lifetime risk in men is ~1 in 23. Screening reduces deaths by 50–60% by finding precancerous polyps early. |
| Lifestyle Risk | Obstructive sleep apnea screening (STOP-Bang; home sleep apnea test if high risk) | Resistant hypertension, cardiovascular strain, and daytime fatigue | Screen once now; repeat if symptoms develop or weight/neck size increases. | An estimated 30–50% of people with hypertension have sleep apnea. Treatment can lower systolic BP by ~2–4 mmHg and improves energy and daytime function. |
| Endocrine | Thyroid-stimulating hormone (TSH) ± free T4 if abnormal | Hypothyroidism contributing to fatigue and adverse lipids | Every 3–5 years, or sooner with fatigue, weight change, cold intolerance, or unexplained high LDL-C. | Thyroid dysfunction affects up to ~5% overt and 5–10% subclinical of adults. Untreated hypothyroidism raises LDL and causes fatigue, impacting cardiovascular risk and energy. |
Recommended Products
Nutrition & Dietary Focus
For a 47-year-old male with hypertension aiming for cardiovascular health, longevity, and steady energy, prioritize a DASH–Mediterranean pattern, keep sodium low, emphasize potassium/magnesium/calcium from foods, raise fiber and omega-3 intake, and be strategic with caffeine, alcohol, and winter vitamin D. These steps are well-aligned with blood pressure control and long-term heart and metabolic health.
Recommendations
Hypertension Management
Adopt a DASH–Mediterranean base: half your plate vegetables/fruit, a quarter whole grains (oats, barley, brown rice), and a quarter lean protein (fish, poultry, legumes); add 1–2 tbsp extra-virgin olive oil and a small handful of unsalted nuts daily. Aim 2–3 servings/day of low-fat dairy or calcium-fortified alternatives.
Hypertension Management
Cap sodium at 1,500–2,000 mg/day. Cook most meals at home; choose “no salt added/low sodium” products; drain and rinse canned goods; flavor with herbs, citrus, vinegar, garlic, and pepper; avoid processed meats, restaurant soups, and salty snacks.
Electrolyte Balance
Boost potassium, magnesium, and calcium from foods: include 4–5 servings/day of potassium-rich produce (leafy greens, beans/lentils, squash, avocado, banana), 1–2 oz/day unsalted nuts/seeds, and 2–3 servings/day low-fat dairy or fortified soy. Avoid potassium-based salt substitutes unless cleared by your clinician.
Cardiovascular Health
Eat fatty fish (salmon, sardines, trout, mackerel) 2–3 times/week. If intake is low, consider an EPA+DHA omega-3 supplement providing ~1–2 g/day after reviewing medications (especially anticoagulants) with your clinician.
Longevity
Target 30–40 g fiber/day from oats/barley, beans/lentils (1 cup most days), vegetables, berries, and chia/flax. If falling short, add 5–10 g/day psyllium with water, increasing gradually.
Energy & Vascular Function
Include nitrate-rich vegetables daily (spinach, arugula, beetroot). For a BP/energy boost around workouts, consider 250–500 mL beet juice or ~3–6 g beet powder 1–2 hours prior if tolerated.
Energy & Metabolic Balance
Distribute protein at ~1.0–1.2 g/kg/day (e.g., 25–35 g per meal) from fish, poultry, legumes, Greek yogurt/soy, and nuts/seeds; pair with high-fiber carbs and healthy fats for stable energy.
Lifestyle Factors for BP & Energy
Limit alcohol to 0–1 drink/day and avoid binge drinking. Keep caffeine ≤300 mg/day and avoid it after early afternoon; prioritize water and unsweetened tea/coffee. In Chicago winters, test 25(OH)D and consider 1,000–2,000 IU vitamin D3/day if low, ideally with magnesium-rich foods.
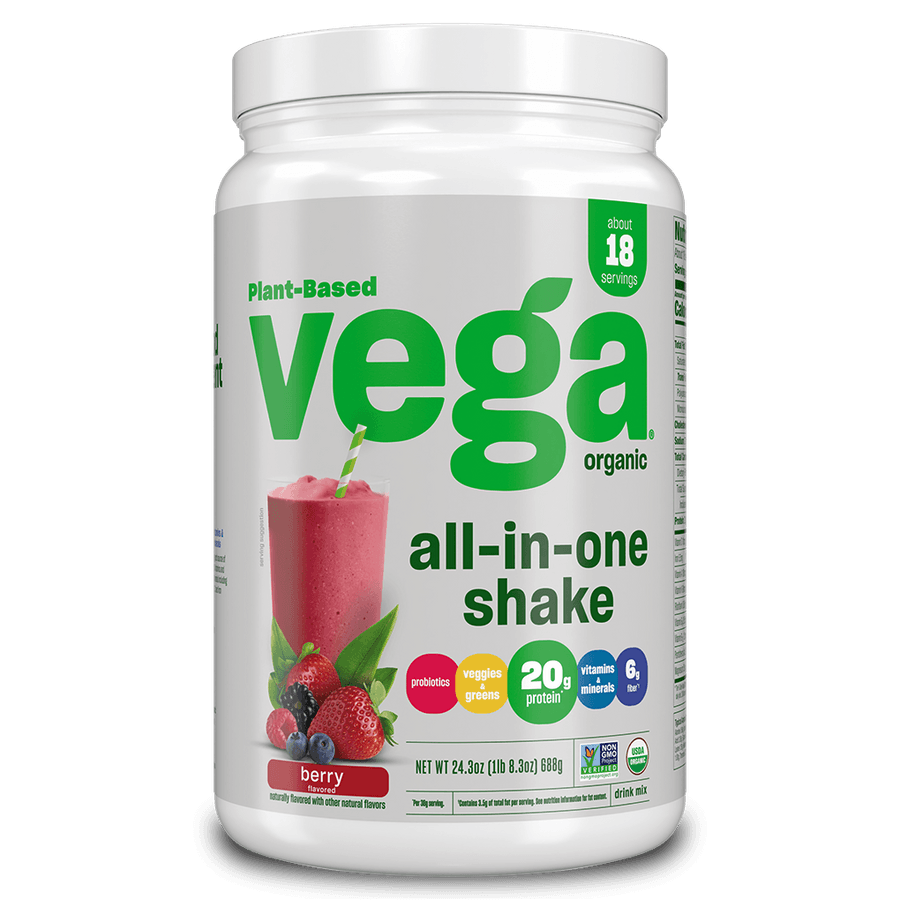
Recommended Products
Supplement Strategy
For a 47-year-old male with hypertension aiming for cardiovascular health, longevity, and steady energy, this stack targets blood pressure control, vascular function, lipid management, and mitochondrial efficiency. Omega-3s, aged garlic, beetroot nitrate, and magnesium address BP and arterial health; CoQ10 and creatine support cellular energy; vitamin D3 supports longevity and metabolic health in northern climates; and psyllium improves cardiometabolic markers.
Supplement Recommendations
Omega-3 (EPA/DHA)
•Cardiovascular Health1,000–2,000 mg combined EPA+DHA daily with meals (fish oil or algae oil).
Magnesium (glycinate or taurate)
•Blood Pressure Support200–400 mg elemental magnesium nightly.
Coenzyme Q10 (ubiquinol)
•Energy & Mitochondrial Health100–200 mg daily with a fat-containing meal.
Vitamin D3
•Longevity1,000–2,000 IU daily with food; adjust to keep 25(OH)D in the optimal range.
Aged Garlic Extract
•Blood Pressure Support1.2 g/day in divided doses (e.g., 2×600 mg).
Beetroot (dietary nitrates)
•Blood Pressure & Exercise PerformanceBeetroot powder or juice standardized to provide ~300–400 mg nitrate daily, ideally 2–3 hours before activity.
Psyllium Husk Fiber
•Cardiometabolic Health6–10 g/day in 1–2 doses with plenty of water, before meals.
Creatine Monohydrate
•Energy & Healthy Aging3–5 g daily (no loading required), powder mixed in water.
Recommended Products
Gut Health & Microbiome
For a 47-year-old man with hypertension in Chicago aiming for cardiovascular health, longevity, and steady energy, prioritize a diverse, fiber-rich microbiome, low-salt gut habits, and a steady gut–brain routine. Emphasize plant variety and fermented foods (low-sodium), meal timing that supports motility, stress/sleep rhythms, and gut-focused strategies that lower inflammatory tone and trim BP-related metabolites (like TMAO).
Recommendations
Microbiome Diversity
Aim for 30+ different plant foods per week with emphasis on prebiotic-rich choices (onions, garlic, leeks, asparagus, Jerusalem artichoke) and pulses; use frozen produce in winter and add resistant starch by cooling cooked potatoes, rice, or oats before eating.
Fermented Foods (Hypertension-Aware)
Include 1–2 daily servings of fermented foods but choose low-sodium options (plain kefir or yogurt, tempeh; rinse jarred sauerkraut/kimchi or pick low-sodium brands).
Salt–Microbiome Link
Keep added salt modest and flavor with herbs, citrus, vinegar, and spices; be mindful that many pickled/fermented products are salty and opt for low-sodium versions.
Gut–Brain Axis for Energy and BP
Build a daily routine: 20–30 minutes of brisk walking—ideally after meals—plus a 10-minute breathing or relaxation practice and consistent 7–8 hour sleep schedule; get morning daylight when possible, even in winter.
Digestive Function & Motility
Space meals 3–4 hours apart and aim for a 12-hour overnight fast with an earlier, lighter dinner; chew thoroughly and avoid late-night snacking.
Cardiometabolic Metabolites (TMAO)
Limit frequent servings of red/processed meats and large egg-yolk-heavy meals; favor fish and plant proteins and include fiber-rich sides when eating meat.
Anti-inflammatory, Microbe-Feeding Polyphenols
Add daily polyphenol sources—berries, green tea, colorful veggies, and extra-virgin olive oil; pair them with fiber-rich meals.
Recommended Products
Energy
Boost daytime energy safely while supporting blood pressure by anchoring your circadian rhythm, using BP‑friendly activity, DASH‑style nutrition, smart caffeine limits, stress downshifts, and better sleep with appropriate medical checks.
Recommendations
Morning light and daily rhythm
Within 60 minutes of waking, get 20–30 minutes of outdoor light; in Chicago winters, use a 10,000‑lux light box at arm’s length for 20–30 minutes. Keep a consistent sleep/wake window and dim screens/lights the last 2 hours before bed.
BP‑smart activity plan
Accumulate 150–300 minutes/week of brisk walking or cycling plus 2 days/week of moderate‑load strength (8–12 reps, avoid breath‑holding). Add 10‑minute brisk walks after meals. On icy/cold days, use indoor options (treadmill, mall/indoor track).
DASH‑style fueling and hydration
Follow a DASH pattern: vegetables/fruit (8–10 servings/day), lean proteins (25–30 g/meal), beans/whole grains, nuts/seeds. Keep sodium ≤1,500–2,000 mg/day; choose potassium‑rich foods unless your clinician has restricted potassium. Hydrate 2–3 L/day; if needed, use low‑sodium electrolytes (<300 mg/L).
Caffeine and stimulant safety
Limit caffeine to 200–300 mg/day and avoid after 12–1 pm. Choose coffee/tea over energy drinks. Avoid stimulants that can raise blood pressure (yohimbine, synephrine, many “fat burners,” and decongestants like pseudoephedrine). Monitor how your BP responds to caffeine.
Stress downshifts (for energy and BP)
Do 5 minutes, 2–3 times/day, of slow breathing (5–6 breaths/min) or a 10‑minute mindfulness session; add hourly 2‑minute movement breaks. Consider an HRV‑biofeedback app/device if helpful.
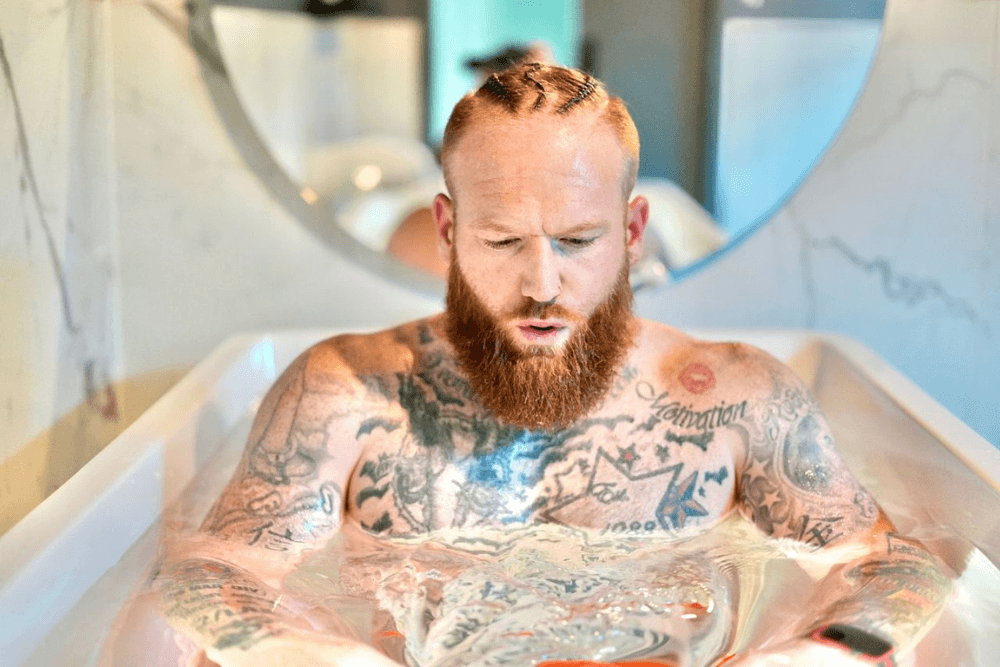
Sleep and medical check for fatigue
Aim for 7–8.5 hours/night; keep the bedroom cool, dark, and quiet; limit alcohol to ≤1 drink/day and avoid within 3 hours of bed. If you snore, have morning headaches or daytime sleepiness, or BP remains elevated, ask about a sleep apnea evaluation. Discuss labs (CBC, ferritin, B12, TSH, vitamin D, A1C) and medication timing with your clinician. Consider CoQ10 100–200 mg with a meal and magnesium glycinate 200–300 mg in the evening only with clinician approval.
Recommended Products
Longevity
At 47 with hypertension, maximizing longevity centers on excellent blood pressure control, cardio-protective eating, consistent exercise that builds VO2max and strength, restorative sleep/stress regulation, and on-time preventive care—while adapting to Chicago’s seasons to keep routines sustainable and energy steady.
Recommendations
Blood pressure mastery
Use an upper‑arm automated cuff and measure BP seated after 5 minutes of rest, morning and evening, 3–4 days/week for two weeks each month; aim for <130/80 mmHg if tolerated; take medications consistently and share your log with your clinician to optimize treatment.
Cardioprotective eating (DASH–Mediterranean)
Center meals on vegetables, fruits, legumes, nuts, whole grains, olive oil, and fish ≥2x/week; keep sodium ≤1,500–2,000 mg/day by limiting processed foods; target ≥30–40 g fiber/day; include potassium‑rich foods (leafy greens, beans) unless your clinician restricts potassium.
Exercise for longevity and energy
Accumulate 150–300 minutes/week of moderate aerobic activity (e.g., brisk walking, cycling) plus 2–3 days/week of resistance training for all major muscle groups; add 4–10 short HIIT intervals once or twice weekly after medical clearance; aim for 7,000–10,000 steps/day; in Chicago winters, warm up indoors and layer to protect from cold.
Sleep and stress regulation
Keep a consistent 7–9‑hour sleep schedule in a dark, cool room; avoid caffeine after noon and alcohol near bedtime; practice 10 minutes daily of slow breathing or mindfulness; consider CBT‑I if insomnia persists.
Preventive care and screenings
At your annual visit, review ASCVD risk, lipids (consider non‑HDL or ApoB), A1c/fasting glucose, kidney function, and medications; start colorectal cancer screening now (age 47); stay current with vaccines (flu yearly, COVID‑19 boosters, Tdap every 10 years), and plan for shingles vaccine at 50.
Smart additions (alcohol, tobacco, nutrients)
If you drink, cap intake at ≤1 drink/day and avoid binges; avoid all tobacco/vaping; during low‑sun months in Chicago, ask about checking vitamin D and consider 1,000–2,000 IU/day D3 if low; if fish intake is low, consider 1–2 g/day EPA+DHA; magnesium glycinate 200–400 mg at night may aid sleep and BP—confirm safety with your clinician, especially with kidney disease or certain medications.
Recommended Products
Cardiovascular Health
For a 47-year-old man with hypertension in Chicago, prioritize lowering blood pressure, heart-healthy eating, consistent indoor-friendly cardio plus strength training, and better sleep/stress control. Pair lifestyle steps with home BP tracking and risk-factor labs to cut cardiovascular risk, support longevity, and improve daily energy.
Recommendations
Blood Pressure Control
Use a validated upper-arm home monitor: take 2 readings morning and evening for 5–7 days each month (seated, feet flat, arm at heart level), average the results, and share with your clinician. Aim for <130/80 mmHg if tolerated; take medications as prescribed; avoid decongestants with pseudoephedrine and routine NSAIDs; if snoring or daytime sleepiness are present, ask about sleep apnea screening.
Heart-Healthy Nutrition (DASH–Mediterranean)
Base meals on vegetables, fruits, beans, nuts, whole grains, fish 2x/week, and olive oil; limit processed meats, refined carbs, and added sugars. Keep sodium near 1,500–2,000 mg/day; prioritize potassium-rich foods unless restricted by your clinician. In Chicago dining, request low-sodium options and watch high-salt items like deli meats, pizza, and soups.
Aerobic and Resistance Training
Accumulate 150–300 minutes/week of moderate cardio (brisk indoor walking, treadmill, cycling, swimming) plus 2 days/week of full-body resistance training; include 7,000–10,000 steps/day. In cold weather, warm up indoors and avoid sudden heavy snow shoveling—use shorter, lighter bouts or a snow blower.
Sleep and Stress
Aim for 7–9 hours/night with a consistent schedule, dark cool bedroom, and no caffeine after 2 pm. Practice 10–15 minutes/day of relaxation (paced breathing, mindfulness, or HRV biofeedback). If you have loud snoring, witnessed apneas, or morning headaches, discuss a sleep study.
Lipids and Metabolic Risk
At your next visit, review a fasting lipid panel (consider ApoB), A1c, and hs-CRP. Discuss statin therapy if your 10-year ASCVD risk is elevated for your age or LDL is high. Favor oily fish and fiber-rich foods; consider fish oil only if triglycerides are elevated, per clinician guidance.
Weight, Alcohol, and Tobacco
If waist circumference is over 40 inches, target a 5–10% weight reduction with adequate protein (about 1.0–1.2 g/kg/day) and a modest calorie deficit. Avoid tobacco/vaping. Limit alcohol to no more than 1 drink/day; less is better for BP.