Workup Health Guide
Personalized wellness insights powered by Workup’s AI — designed to help you explore health solutions aligned with your goals.
Profile Overview
Disclaimer: This report was produced using Workup’s AI recommendation engine, which evaluates your demographic and health information to identify potentially relevant products and services from vetted partners. Workup does not practice medicine, and this content is for informational purposes only. Consult your physician or licensed practitioner before making any healthcare decisions.
Overview
This personalized guide offers a preventive health plan for a 35-year-old female in Los Angeles, CA, managing PCOS. It focuses on hormone balance, fertility support, and energy improvement.
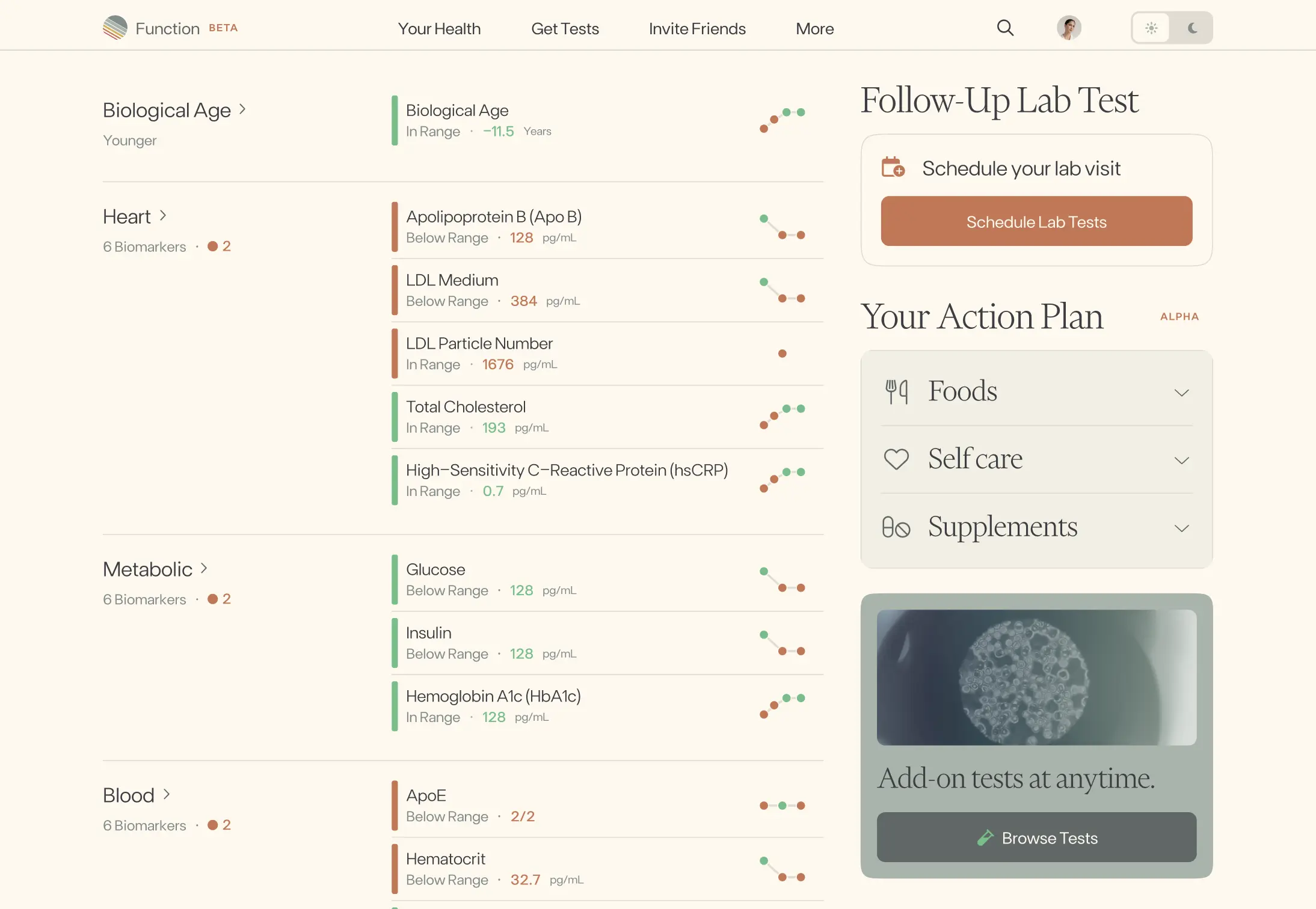
Diagnostics & Screenings
For a 35-year-old woman with PCOS aiming for hormone balance, fertility support, and better energy, prioritize cardiometabolic risk detection (glucose intolerance, lipids, blood pressure), reproductive and thyroid hormone assessment, and key age-appropriate cancer and lifestyle screenings. Start with a comprehensive baseline, then monitor more frequently when abnormal, symptomatic, or while trying to conceive. This plan targets common PCOS comorbidities (insulin resistance, dyslipidemia, thyroid dysfunction, sleep apnea), addresses ovulation and androgen excess, and checks reversible causes of fatigue such as iron deficiency.
Screening Overview
| Tier | Test | Risk Area | Frequency | Why It Matters |
|---|---|---|---|---|
| Cardiovascular | Fasting lipid panel (LDL, HDL, triglycerides, non-HDL) | Atherosclerotic cardiovascular disease risk in PCOS | Get a baseline now; repeat every 1–3 years if normal, or annually if abnormal, on therapy, or planning pregnancy with metabolic risk. | Up to 60–70% of women with PCOS have lipid abnormalities, and heart disease remains the leading cause of death; early treatment lowers long-term risk. |
| Metabolic | Glucose tolerance screening (A1C plus 75‑g 2‑hour OGTT) | Insulin resistance, prediabetes, and type 2 diabetes | At baseline; then every 1–3 years. Test yearly if you have overweight, strong family history, prior gestational diabetes, or symptoms. | PCOS raises type 2 diabetes risk about 4×; up to ~40% have impaired glucose tolerance by age 40—detecting it early prevents progression. |
| Organ Function | Comprehensive metabolic panel (electrolytes, kidney function, liver enzymes) | Nonalcoholic fatty liver disease and medication safety | Annually if stable; every 6 months if on metformin, statins, or if prior abnormalities. | Fatty liver affects ~25% of adults and is more common in PCOS; catching liver or kidney issues early prevents complications and guides safe medication use. |
| Endocrine/Thyroid | Thyroid function (TSH with reflex free T4) and TPO antibodies if trying to conceive or with symptoms | Hypothyroidism/hyperthyroidism impacting fertility and energy | Baseline and preconception; then every 1–2 years or sooner if symptoms arise or on thyroid medication. | About 1 in 8 women develop thyroid disease; untreated hypothyroidism increases infertility and miscarriage risk and can cause fatigue and mood changes. |
| Hormonal (PCOS) | Androgen profile (total and free testosterone, SHBG, and DHEAS) | Hyperandrogenism driving cycle irregularity, acne/hair changes, and ovulatory dysfunction | Every 6–12 months while managing PCOS, or sooner if symptoms change or medications are adjusted. | Clinical or biochemical hyperandrogenism is present in ~70–80% of PCOS; tracking androgens helps tailor therapy and improve symptoms and fertility. |
| Fertility | Ovulation confirmation (mid‑luteal serum progesterone or validated LH ovulation kits) | Anovulation contributing to infertility | Each cycle while trying to conceive; otherwise 1–2 times per year to assess ovulatory status. | PCOS accounts for up to 80% of anovulatory infertility; confirming ovulation guides timing of intercourse and treatment escalation if needed. |
| Hematology/Energy | Complete blood count (CBC) and ferritin (iron stores) | Iron deficiency anemia causing fatigue and reduced exercise tolerance | Annually, or sooner with heavy periods, fatigue, hair loss, or dietary risk (e.g., vegetarian). | Iron deficiency affects roughly 10% of U.S. women; low ferritin is a common, reversible cause of fatigue and impaired cognition. |
| Inflammation/Cardiovascular Risk | High‑sensitivity C‑reactive protein (hs‑CRP) | Systemic inflammation and cardiovascular risk stratification | Baseline with other risk labs; then every 2–3 years, or yearly if additional risk factors are present. | People with elevated hs‑CRP have about 2× higher risk of heart attack and stroke; low‑grade inflammation is common in PCOS and responds to lifestyle change. |
| Cancer (Age‑Appropriate) | Cervical cancer screening (Pap + HPV co‑test) | Cervical dysplasia and cancer from high‑risk HPV | Every 5 years with co‑testing at ages 30–65 (or Pap alone every 3 years if preferred). | High‑risk HPV causes >90% of cervical cancers; regular screening can cut incidence and mortality by more than half through early detection and treatment. |
| Risk/Lifestyle | Obstructive sleep apnea screening (questionnaire ± home sleep test if positive) | Sleep apnea worsening insulin resistance, blood pressure, and daytime fatigue | Screen now; repeat if symptoms (snoring, witnessed apneas, daytime sleepiness) develop, with weight changes, or during preconception planning. | Women with PCOS have 2–3× higher sleep apnea risk; treating OSA improves energy, blood pressure, and glucose control. |
Recommended Products
Nutrition & Dietary Focus
Personalized plan for a 35-year-old woman with PCOS focused on stabilizing blood sugar to balance hormones, supporting ovulation and egg quality for fertility, and improving steady energy through a Mediterranean, low‑glycemic pattern plus targeted micronutrients.
Recommendations
Metabolic Balance & Hormone Regulation
Center meals on a Mediterranean, low‑glycemic plate: ~50% non‑starchy vegetables, 25% lean protein, 25% slow carbs (beans, lentils, intact whole grains, sweet potato), plus 1–2 Tbsp extra‑virgin olive oil. Aim for 30–40 g fiber/day and keep added sugars <25 g/day.
Protein Optimization
Target ~1.2–1.6 g protein/kg/day (spread across meals with 25–35 g at breakfast and lunch). Choose fish, eggs, Greek yogurt, tofu/tempeh, poultry, and legumes; pair carbs with protein and fat at every meal/snack.
Inositol for PCOS & Fertility
Use a myo‑inositol:D‑chiro‑inositol 40:1 blend (e.g., 2 g myo + 50 mg D‑chiro twice daily with meals) for 3–6 months; continue while trying to conceive and confirm with your clinician once pregnant. If you take metformin, this combo is commonly used alongside it.
Omega‑3s & Anti‑Inflammatory Fats
Eat 2–3 servings/week of low‑mercury fatty fish (salmon, sardines, trout) or take 1–2 g/day combined EPA+DHA (algal DHA if plant‑based). Limit fried foods and refined seed oils; use extra‑virgin olive oil and include nuts/seeds daily.
Vitamin D & Prenatal Micronutrients
Check 25‑OH vitamin D; typically supplement 1,000–2,000 IU D3/day to reach 30–50 ng/mL. In sunny Los Angeles, brief morning sun (10–15 min to arms/legs, then apply SPF) can help. Start a prenatal with methylfolate (400–800 mcg), iodine (150 mcg), choline (~450 mg), and B12; use iron only if labs indicate need.
Smart Carbohydrate Timing, Caffeine & Alcohol
Time most carbs earlier in the day and around activity; pair all carbs with protein/fat. Keep a gentle 12‑hour overnight fast. If trying to conceive, keep caffeine ≤200 mg/day and minimize alcohol; avoid high‑mercury fish (swordfish, king mackerel, tilefish, bigeye tuna).
Magnesium & Sleep Support
Include magnesium‑rich foods (pumpkin seeds, almonds, leafy greens, beans) and consider magnesium glycinate 200–400 mg in the evening as tolerated; aim for 7–9 hours of consistent sleep in a cool, dark room.
Gut Health & Helpful Botanicals
Eat 6–9 servings/day of colorful produce and include fermented foods (yogurt/kefir, sauerkraut) most days. Consider Ceylon cinnamon 1–2 g/day with meals and spearmint tea 1–2 cups/day.
Recommended Products
Supplement Strategy
For a 35-year-old woman with PCOS aiming for hormone balance, fertility, and better energy, prioritize insulin-sensitizing and ovulation-supportive nutrients (inositols, NAC, vitamin D3), mitochondrial and anti-inflammatory support (CoQ10, omega-3s), and foundational preconception coverage (prenatal) with gentle stress/sleep support (magnesium). These choices are evidence-based for PCOS and appropriate when trying to conceive.
Supplement Recommendations
Myo‑Inositol + D‑Chiro‑Inositol (40:1)
•Hormone Balance & Ovulation2 g myo‑inositol + 50 mg D‑chiro‑inositol twice daily (powder or capsules)
N‑Acetyl‑Cysteine (NAC)
•Fertility Support & Antioxidant Defense600 mg, 2–3 times daily
Omega‑3 (EPA/DHA) from fish oil or algae
•Inflammation & Fertility1,000–2,000 mg per day of combined EPA+DHA with food
Vitamin D3
•Hormone & Metabolic Health1,000–2,000 IU daily (adjust to 25‑OH vitamin D levels)
CoQ10 (prefer ubiquinol)
•Energy & Mitochondrial Support100–200 mg daily with a meal containing fat
Magnesium (glycinate or bisglycinate)
•Sleep, Stress & Metabolic Support200–300 mg elemental magnesium in the evening
Prenatal multivitamin (with methylfolate)
•Preconception FoundationDaily prenatal providing 400–800 mcg methylfolate, 150 mcg iodine, plus B12 and choline; DHA may be separate
Probiotic (Lactobacillus/Bifidobacterium blend)
•Gut–Metabolic Axis10–20 billion CFU daily
Recommended Products
Gut Health & Microbiome
For a 35-year-old woman with PCOS aiming for hormone balance, fertility support, and better energy, prioritize: 1) diversifying gut microbes to boost SCFAs and insulin sensitivity, 2) supporting the gut–brain axis for steadier cortisol and appetite signals, 3) optimizing digestion and motility, 4) calming gut-driven inflammation, and 5) promoting healthy estrogen metabolism via the estrobolome.
Recommendations
Microbiome Diversity
Aim for ~30 different plant foods per week, including prebiotic-rich choices (onion, garlic, leeks, asparagus, Jerusalem artichoke) and 1 small serving of resistant starch most days (cooked–cooled potatoes or rice, green banana flour, or lentils). Use LA farmers’ markets for variety.
Fermented Foods & Probiotics
Include 1–2 daily servings of fermented foods (plain yogurt or kefir, sauerkraut/kimchi, tempeh, miso). If foods are limited, consider a 8–12 week trial of a multi‑strain Lactobacillus/Bifidobacterium probiotic; continue if you notice improved regularity, less bloating, or better energy. If pregnant or trying to conceive, review with your clinician.
Gut–Brain Axis
Before meals, do 2–3 minutes of slow breathing (about 6 breaths/min) or humming to activate the vagus nerve; take a relaxed 10‑minute walk after meals; keep a consistent sleep window.
Digestive Function
Practice meal hygiene: chew thoroughly, avoid constant grazing, and leave 3–4 hours between meals to allow the migrating motor complex; finish dinner 2–3 hours before bed. Use ginger or peppermint tea for occasional bloating; if symptoms persist, consider a short, guided low‑FODMAP trial with reintroduction.
Inflammation & Gut Barrier
Cook with extra‑virgin olive oil and add colorful polyphenol sources daily (berries, herbs, green tea) plus turmeric with a pinch of black pepper; include soluble fibers like oats or chia.
Estrobolome & Hormone Metabolism
Reach 25–35 g fiber/day and add 1–2 Tbsp ground flaxseed plus regular cruciferous vegetables (broccoli, cabbage, arugula). Keep bowels regular; limit alcohol to support microbial balance.
Recommended Products
Hormone Balance
For a 35-year-old woman in Los Angeles with PCOS, the fastest wins for hormone balance focus on improving insulin sensitivity and lowering androgen excess: low-glycemic, protein- and fiber-forward meals; consistent strength + cardio; restorative sleep and stress regulation; evidence-based supplements (inositol, omega-3, vitamin D, magnesium); and cycle/lab monitoring with your clinician to personalize care and support fertility and energy.
Recommendations
Low-Glycemic, Anti-Inflammatory Plate
At each meal, include 25–35 g protein (eggs, fish, tofu, poultry), a fist of high‑fiber carbs (beans, quinoa, berries) plus 2+ cups non‑starchy veggies, and healthy fats (olive oil, avocado). Limit added sugars/refined grains; aim for 30–40 g fiber/day and a consistent 12‑hour overnight fast; keep meal timing regular.
Strength + Cardio Routine
Do full‑body resistance training 2–4 days/week (6–10 compound moves, 2–3 sets) and 150–300 min/week of brisk walking/cycling; add 1–2 short interval sessions if well‑recovered. Build in 1–2 easy days weekly.
Evidence‑Based Supplements for PCOS
Consider myo‑inositol 2000 mg + D‑chiro‑inositol 50 mg twice daily (40:1 ratio); omega‑3 (EPA+DHA) 1–2 g/day with meals; vitamin D3 per labs (often 1000–2000 IU/day if not tested); magnesium glycinate 200–400 mg in the evening. Confirm with your clinician, especially if pregnant, trying to conceive, or on medications.
Sleep Optimization
Target 7–9 hours nightly with a fixed sleep/wake window; dim screens 1–2 hours pre‑bed, keep the room cool/dark, and avoid caffeine after noon and alcohol on weeknights.
Stress Regulation & Light/Walks
Practice 10–15 minutes/day of mindfulness, box breathing (4‑4‑4‑4), or yoga; get morning outdoor light and add 5–10 minute walks after meals.
Cycle & Lab Monitoring with Clinician
Track cycle length, ovulation signs, and symptoms. Ask about labs: fasting glucose/insulin or OGTT, A1c, lipid panel, TSH, prolactin, 25‑OH vitamin D, total/free testosterone, DHEAS, SHBG. Discuss options if cycles stay irregular or when TTC.
Recommended Products
Fertility Support
Primary aim: improve ovulation quality and timing in PCOS while supporting hormone balance and steady energy. Focus on insulin sensitivity, targeted micronutrients, smart cycle tracking, and restorative lifestyle habits, with medical coordination if conception does not occur within 6 months at age 35+.
Recommendations
Insulin-sensitizing nutrition
Adopt a low‑glycemic, Mediterranean-style plate at each meal: fill half with non‑starchy vegetables, a palm of lean protein, 1–2 thumbs of olive oil/avocado/nuts, and a fist of high‑fiber carbs (e.g., beans, quinoa, berries). Distribute carbs evenly, target 25–35 g fiber/day, and add a 10–15 minute walk after meals.
Core preconception micronutrients
Begin a prenatal with 400–800 mcg methylfolate, 150 mcg iodine (if not on thyroid-blocking meds), 400–450 mg choline, and 200–300 mg DHA; choose iron only if you’ve been advised or are iron‑deficient. Ask your clinician to check vitamin D and supplement if low.
PCOS-targeted supplements
Discuss using myo‑inositol plus D‑chiro‑inositol (commonly 2 g/40 mg twice daily to approximate a 40–50:1 ratio). Consider omega‑3s providing ~1 g/day EPA+DHA. Coordinate all supplements with your OB‑GYN before or during attempts to conceive.
Training for ovulation and energy
Aim for 150–300 minutes/week of moderate cardio plus 2–3 days/week of strength training; include brief post‑meal walks. If doing HIIT, keep to 1–2 short sessions/week and prioritize recovery and sleep (7–9 hours/night).
Cycle tracking and timing
Track basal body temperature and cervical mucus; use ovulation predictor kits cautiously (PCOS can give false positives). Time intercourse every 1–2 days in the fertile window; consider mid‑luteal progesterone testing to confirm ovulation and use fertility‑friendly lubricant if needed.
Medical coordination and lifestyle essentials
At age 35, seek preconception care: request labs (TSH, A1c/fasting glucose, lipids, vitamin D, prolactin) and discuss options like letrozole for ovulation induction if not pregnant after 6 months. Limit caffeine to ≤200 mg/day and alcohol to minimal/occasional; avoid smoking and reduce endocrine disruptors (avoid heating food in plastic, choose fragrance‑free/home products).
Recommended Products
Energy Improvement
Focus on steady energy for a 35-year-old woman with PCOS and fertility goals by stabilizing blood sugar, optimizing sleep/circadian rhythm, using caffeine and hydration wisely, moving strategically, managing stress, and checking key nutrients.
Recommendations
Blood sugar stability for sustained energy
Build every meal with protein (25–30 g at breakfast), fiber-rich carbs, and healthy fats; eat on a regular cadence (about every 3–4 hours). Start the day with a protein-forward breakfast within 60–90 minutes of waking.
Circadian rhythm and sleep quality
Get 5–15 minutes of outdoor morning light within an hour of waking (easy year-round in Los Angeles). Aim for 7.5–9 hours of sleep, keep a consistent schedule, stop screens 60 minutes before bed, and keep the bedroom cool and dark.
Smart caffeine and hydration
Limit caffeine to ≤200 mg/day (safer for fertility), finish by noon, and have it with or after breakfast—not on an empty stomach. Hydrate with 2–2.5 L water daily; on hot LA days or workouts, add electrolytes without added sugar.
Targeted movement for energy
Take 10–15 minute brisk walks after 1–2 meals most days and do 2–3 short resistance sessions per week (20–30 minutes, full-body). Add 3–5 minute “movement snacks” each hour you’re sedentary.
Stress modulation and micro-recovery
Schedule 1–2 daily mini-breaks (5–10 minutes) for breathwork (e.g., 4-7-8), mindfulness, or a brief outdoor walk. Create a 10–15 minute wind-down routine in the evening.
Check key nutrients; consider gentle support
Ask your clinician about testing CBC, ferritin/iron, vitamin B12, vitamin D, and thyroid (TSH/free T4). If appropriate, consider a prenatal with methylfolate and B12, and magnesium glycinate 200–300 mg in the evening (confirm with your provider).