Workup Health Guide
Personalized wellness insights powered by Workup’s AI — designed to help you explore health solutions aligned with your goals.
Profile Overview
Disclaimer: This report was produced using Workup’s AI recommendation engine, which evaluates your demographic and health information to identify potentially relevant products and services from vetted partners. Workup does not practice medicine, and this content is for informational purposes only. Consult your physician or licensed practitioner before making any healthcare decisions.
Overview
This guide is tailored for a 72-year-old male living in NYC with diagnoses of heart disease and vertigo. It focuses on preventive measures and strategies to promote heart health and manage vertigo, with a personal goal of supporting hair growth.
Diagnostics & Screenings
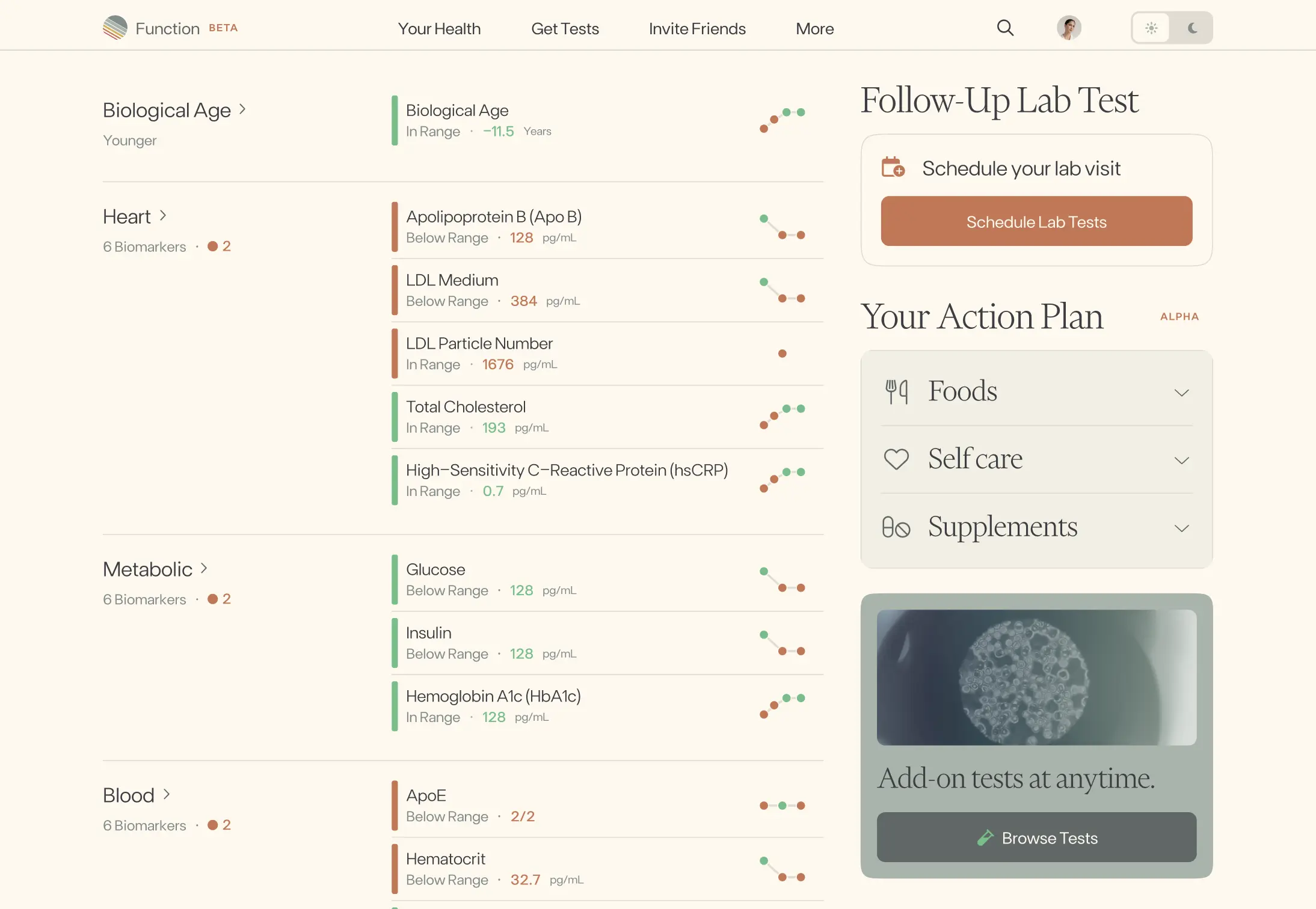
At 72 with established heart disease and vertigo, the plan prioritizes cardiovascular risk control, metabolic disease detection, organ-function safety labs for cardiac medications, and age-appropriate cancer screening. We also address hair-loss contributors (thyroid and iron) and vertigo-related fall risk. Most tests are annual, with tighter intervals when medications change or results are abnormal. Shared decision-making is used for PSA at your age, and colorectal screening continues if overall health/life expectancy remains good.
Screening Overview
| Tier | Test | Risk Area | Frequency | Why It Matters |
|---|---|---|---|---|
| Cardiovascular | Blood pressure monitoring | Hypertension driving stroke and heart-attack risk | Check at every clinic visit and at home 1–2 times per week; escalate care if readings stay above ~130/80 mmHg. | About 1 in 2 U.S. adults has high blood pressure, and each 20/10 mmHg rise roughly doubles risk of cardiovascular death. |
| Cardiovascular | Advanced lipid panel with ApoB and Lp(a) | Atherosclerotic event risk and residual risk from Lp(a) | At least yearly; recheck 6–12 weeks after any statin/ezetimibe/PCSK9 change. Measure Lp(a) once in a lifetime (or when considering targeted therapy). | Lowering LDL-C by ~39 mg/dL reduces major vascular events by ~20–25%. Elevated Lp(a) occurs in about 1 in 5 adults and independently raises heart-attack and stroke risk. |
| Metabolic | A1C and fasting glucose | Diabetes and prediabetes affecting cardiovascular outcomes | Every 6–12 months; sooner if weight, diet, or medications change, or if symptoms of diabetes appear. | Nearly half of adults ≥65 have prediabetes and about 1 in 4 have diabetes; diabetes roughly doubles cardiovascular risk. |
| Inflammation | hs-CRP (high-sensitivity C-reactive protein) | Residual inflammatory risk in coronary disease | Annually if you have known heart disease or when adjusting therapy that may affect inflammation. | An hs-CRP above 2 mg/L is linked to higher heart attack and stroke risk even with controlled LDL; addressing inflammation can lower events in selected patients. |
| Organ Function | Comprehensive metabolic panel with eGFR and urine albumin | Kidney and liver health, medication safety, and vascular risk | Once a year, and 4–12 weeks after starting or changing heart or blood-pressure medicines (e.g., statins, ACE inhibitors, diuretics). | Chronic kidney disease affects about 1 in 7 adults; albumin in urine signals higher kidney and heart risk, and liver/kidney values guide safe dosing of cardiac drugs. |
| Endocrine | Thyroid panel (TSH ± Free T4) | Hypothyroidism contributing to hair loss, fatigue, and dyslipidemia | Every 1–2 years, or sooner if symptoms such as fatigue, cold intolerance, or hair thinning worsen. | Around 5% of adults have thyroid disease; untreated hypothyroidism can worsen cholesterol and cause diffuse hair shedding that improves when corrected. |
| Nutrition/Hematology | Iron studies with ferritin | Iron deficiency and anemia impacting hair growth and exercise tolerance | Obtain a baseline once; repeat if low, if hair shedding persists, or if there is bleeding risk or new fatigue. | Anemia affects roughly 10% of adults aged ≥65; iron deficiency is a leading reversible cause of hair loss and can worsen cardiovascular symptoms. |
| Cancer | Prostate cancer screening (PSA) — shared decision at age 72 | Prostate cancer detection balanced against overdiagnosis | Discuss whether to continue. If you choose to screen and have a ≥10‑year life expectancy, test every 1–2 years. | About 1 in 8 men develop prostate cancer. USPSTF advises against routine screening after 70, but some healthy men opt to continue to reduce metastatic disease risk. |
| Cancer | Colorectal cancer screening (FIT or colonoscopy) | Early detection and prevention via polyp removal | Continue through age 75 if in good health: FIT every year, or colonoscopy every 10 years (or sooner if prior polyps). | Colorectal cancer is a leading cause of cancer death; screening lowers mortality and prevents cancer by removing precancerous polyps. |
| Risk/Lifestyle | Falls risk and vestibular assessment | Falls and injury related to vertigo and balance problems | At least yearly and after any fall or medication change; include orthostatic blood pressure, Timed Up-and-Go, medication review, and Dix–Hallpike for positional vertigo. | About 1 in 4 adults ≥65 falls each year, a major cause of fractures and hospitalization; benign positional vertigo is common in older adults and is highly treatable with maneuvers and vestibular therapy. |
Recommended Products
Nutrition & Dietary Focus
For a 72-year-old man with heart disease and vertigo aiming for better hair growth, focus on a Mediterranean-style, low-sodium pattern rich in omega-3s, fiber, and plant foods; maintain steady hydration, adequate protein, and check key micronutrients (vitamin D, B12, zinc). Use supplements judiciously with attention to heart-medication interactions and lab-test safety (biotin).
Recommendations
Heart Health (Diet Pattern)
Adopt a Mediterranean-style pattern: half the plate vegetables, a quarter whole grains/legumes, a quarter lean protein; cook with extra-virgin olive oil; eat fatty fish 2–3 times/week; a small handful of unsalted nuts most days; limit red/processed meats, refined grains, and sugary foods.
Sodium, Caffeine, Alcohol (Heart & Vertigo)
Keep sodium at 1,500–2,000 mg/day by minimizing processed/restaurant foods and choosing low-sodium versions; season with herbs, citrus, and vinegar. Limit caffeine to about 1 cup coffee/day and alcohol to ≤1 drink/day or less.
Hydration & Meal Timing (Vertigo Support)
Distribute fluids evenly across the day to total ~8–10 cups (unless your cardiologist set a fluid restriction). Eat smaller, regular meals with balanced carbs and protein; avoid large, very salty meals.
LDL Reduction (Fiber & Sterols)
Aim for 30–40 g/day fiber with 10–15 g soluble fiber from oats, barley, beans/lentils, chia, ground flax, apples, and citrus. Consider 1–2 tsp psyllium husk daily with water and ~2 g/day plant sterols from fortified foods or supplements.
Omega-3s (Heart & Hair)
Choose salmon, sardines, trout, or mackerel 2–3 times/week. If intake is low, discuss a fish oil providing ~1 g/day EPA+DHA with your cardiologist, especially if on blood thinners.
Protein for Healthy Aging & Hair
Target ~1.0–1.2 g protein/kg/day (e.g., ~70–90 g/day if 70–75 kg), spread 25–35 g per meal from fish, legumes, tofu/tempeh, eggs, low-fat dairy, and skinless poultry; consider 10–15 g/day collagen peptides if desired.
Micronutrient Adequacy (Hair & Neurologic)
Ask your clinician to check vitamin D, B12, zinc, ferritin, and thyroid. Maintain vitamin D sufficiency (often 1,000–2,000 IU D3/day in NYC winters), include zinc foods (oysters, pumpkin seeds), and selenium from 1 Brazil nut/day; use fortified foods or a B12 supplement if low. Avoid iron unless prescribed and avoid high-dose biotin.
Supplement & Medication Safety
Keep leafy-green vitamin K intake consistent if on warfarin; avoid grapefruit if on statins or certain heart meds; if anticoagulated, avoid high-dose fish oil, ginger, ginkgo, and turmeric supplements; stop high-dose biotin 48–72 hours before labs.
Recommended Products
Supplement Strategy
For a 72-year-old man with heart disease and vertigo seeking hair growth, emphasize a heart-safe core (omega-3s, ubiquinol CoQ10, vitamin D, magnesium) to support cardiovascular function and vestibular stability, while adding hair-focused nutrients (pumpkin seed oil, collagen + vitamin C). Creatine and B12 round out strength, energy, and healthy aging support—all with conservative, age-appropriate dosing.
Supplement Recommendations
Omega-3 (EPA+DHA)
•Cardiovascular Health1,000 mg/day combined EPA+DHA from high-quality triglyceride-form fish oil, with meals
Coenzyme Q10 (Ubiquinol)
•Cardiovascular Energy & Statin Support100–200 mg/day ubiquinol with a fat-containing meal
Vitamin D3
•Bone/Vestibular & Immune Support1,000–2,000 IU (25–50 mcg) daily, softgel or drops
Magnesium (Glycinate)
•Neuromuscular Calm & Vestibular Support200–300 mg elemental magnesium nightly in glycinate/chelated form
Creatine Monohydrate
•Healthy Aging & Strength3 g/day creatine monohydrate powder, no loading phase, with water or a meal
Pumpkin Seed Oil
•Hair Growth1,000–2,000 mg/day softgels (split doses)
Collagen Peptides + Vitamin C
•Hair/Scalp & Skin Structure5–10 g/day hydrolyzed collagen peptides plus 50–100 mg vitamin C
Vitamin B12 (Methylcobalamin)
•Neurovascular & Energy Support1,000 mcg sublingual tablet, 2–3 times per week
Recommended Products
Gut Health & Microbiome
For a 72-year-old man with heart disease and vertigo aiming for hair growth, prioritize gentle, heart-conscious ways to build microbiome diversity (plant fibers + low-sodium ferments), calm the gut–brain axis to ease post-meal dizziness, optimize digestion/regularity, and lower gut-driven inflammation to support cardiovascular and scalp health. Keep changes gradual to avoid bloating and choose low-sodium options.
Recommendations
Microbiome Diversity
Aim for 30 different plant foods/week, emphasizing resistant starch 3x/week (cooled potatoes or rice, green bananas/plantains) and beta-glucans from oats/barley.
Balanced Gut Function (Fermented Foods)
Include 1 serving/day of low-sodium fermented foods—plain yogurt or kefir, tempeh, or rinsed sauerkraut/kimchi—rotating choices across the week.
Gut–Brain Axis (Vertigo Support)
Before main meals, practice 3–5 minutes of slow diaphragmatic breathing and eat unhurriedly (20–30 minutes), with smaller portions on vertigo days.
Digestive Function
Finish dinner 3+ hours before bed, stay upright or take a gentle 10-minute walk after meals, and elevate the head of the bed 6–8 inches if reflux tends to occur.
Inflammation Modulation
Add polyphenol-rich foods daily (berries, green tea, cocoa, extra-virgin olive oil) paired with fiber at the same meal (e.g., berries with oats).
Balanced Gut Function & Absorption (Hair Goal)
Target 25–30 g/day fiber with 1–2 green kiwifruit or 1–2 tsp psyllium in water for regularity; have probiotic yogurt or kefir with iron/zinc-containing meals and keep tea/coffee 60 minutes away from those meals.
Recommended Products
Hair Growth
For a 72-year-old male with heart disease and vertigo, prioritize safe, evidence-based hair growth strategies: topical minoxidil foam, scalp inflammation control, nutrition and lab optimization, low-level laser therapy, and medication review. Avoid oral minoxidil and high-dose biotin; tailor routines to reduce vertigo risk.
Recommendations
First-line topical therapy
Apply topical minoxidil 5% foam once nightly to thinning scalp areas (about half a capful), let dry fully, and wash hands. Avoid oral minoxidil given your cardiac history. Stop and contact your clinician if you notice chest pain, palpitations, ankle swelling, or significant dizziness.
Scalp health and inflammation control
Use ketoconazole 1% shampoo 2–3 times weekly (leave on 3–5 minutes) and alternate with a gentle sulfate-free shampoo; treat any dandruff or itch promptly. Sit while showering if vertigo is triggered by head movements.
Nutrition and labs for hair support
Ask your doctor to check ferritin, iron/TIBC, vitamin D, B12, and TSH. Aim for 1.0–1.2 g/kg/day of protein via heart-healthy foods (fish, eggs, legumes, Greek yogurt, nuts) plus leafy greens, berries, and olive oil. Supplement only if deficient and avoid high-dose biotin due to interference with cardiac troponin tests.
Low-level laser therapy (LLLT)
Use an FDA-cleared LLLT cap or comb 3–4 days per week for 10–20 minutes, preferably while seated; combine consistently with minoxidil and reassess results after 3–6 months.
Medication and condition review
Book a review with your cardiologist/PCP and a board-certified dermatologist (NYC has several academic hair clinics). Screen for drug-related shedding (e.g., some beta-blockers, statins, anticoagulants, amiodarone) and discuss prescription options like topical or oral finasteride if appropriate with PSA monitoring; avoid saw palmetto if you take antiplatelets/anticoagulants.
Gentle care, stress, and sleep
Avoid tight hats and traction hairstyles; use a wide-tooth comb and a soft pillowcase. Do 5 minutes of gentle seated scalp massage daily and aim for 7–8 hours of sleep with brief daily relaxation breathing, performed seated to reduce vertigo risk.