Workup Health Guide
Personalized wellness insights powered by Workup’s AI — designed to help you explore health solutions aligned with your goals.
Profile Overview
Disclaimer: This report was produced using Workup’s AI recommendation engine, which evaluates your demographic and health information to identify potentially relevant products and services from vetted partners. Workup does not practice medicine, and this content is for informational purposes only. Consult your physician or licensed practitioner before making any healthcare decisions.
Overview
This guide offers a tailored preventive health strategy for a 40-year-old male in Hoboken, NJ, focusing on inflammation reduction and immune support due to Hashimoto’s Disease.
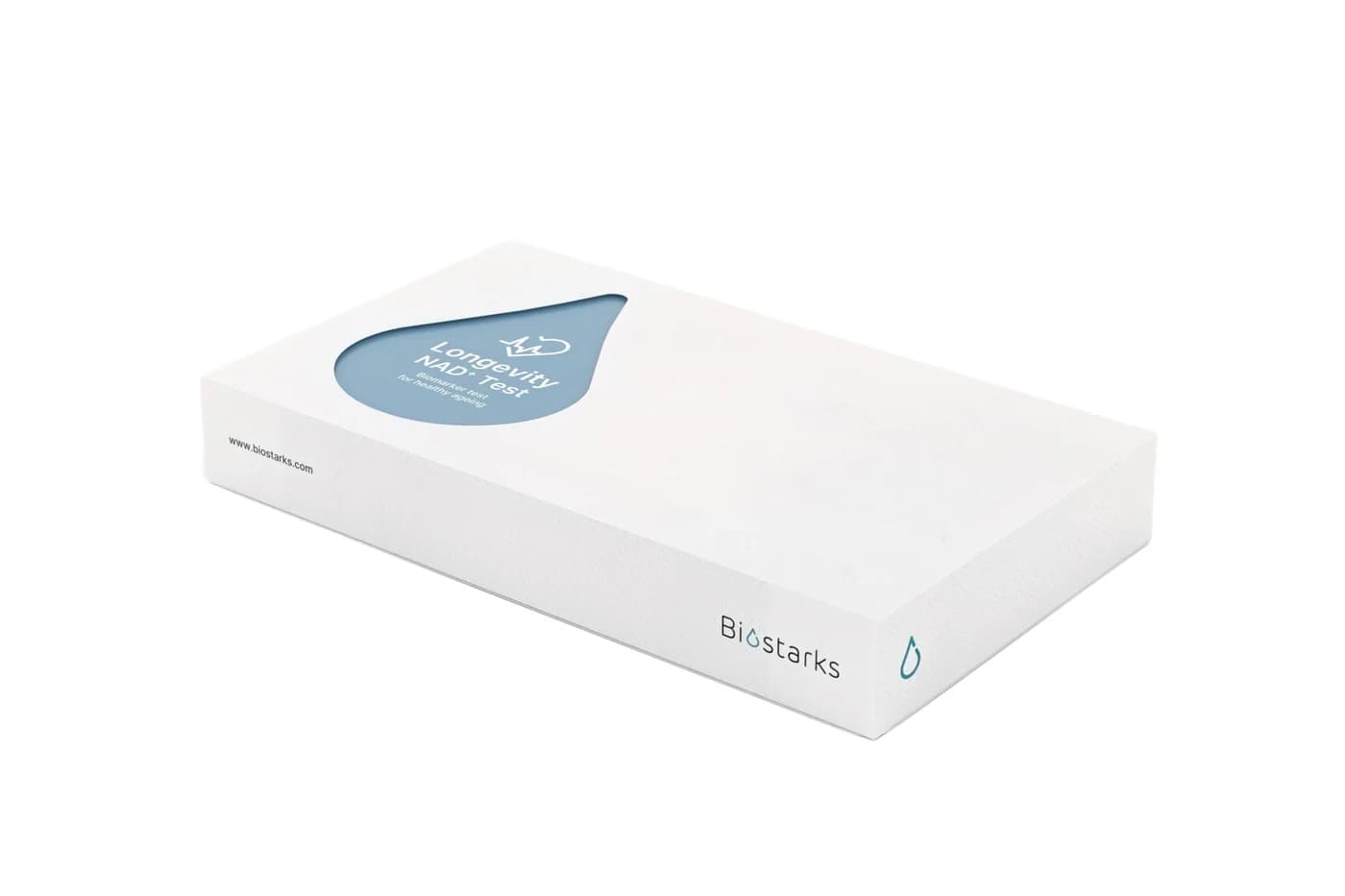
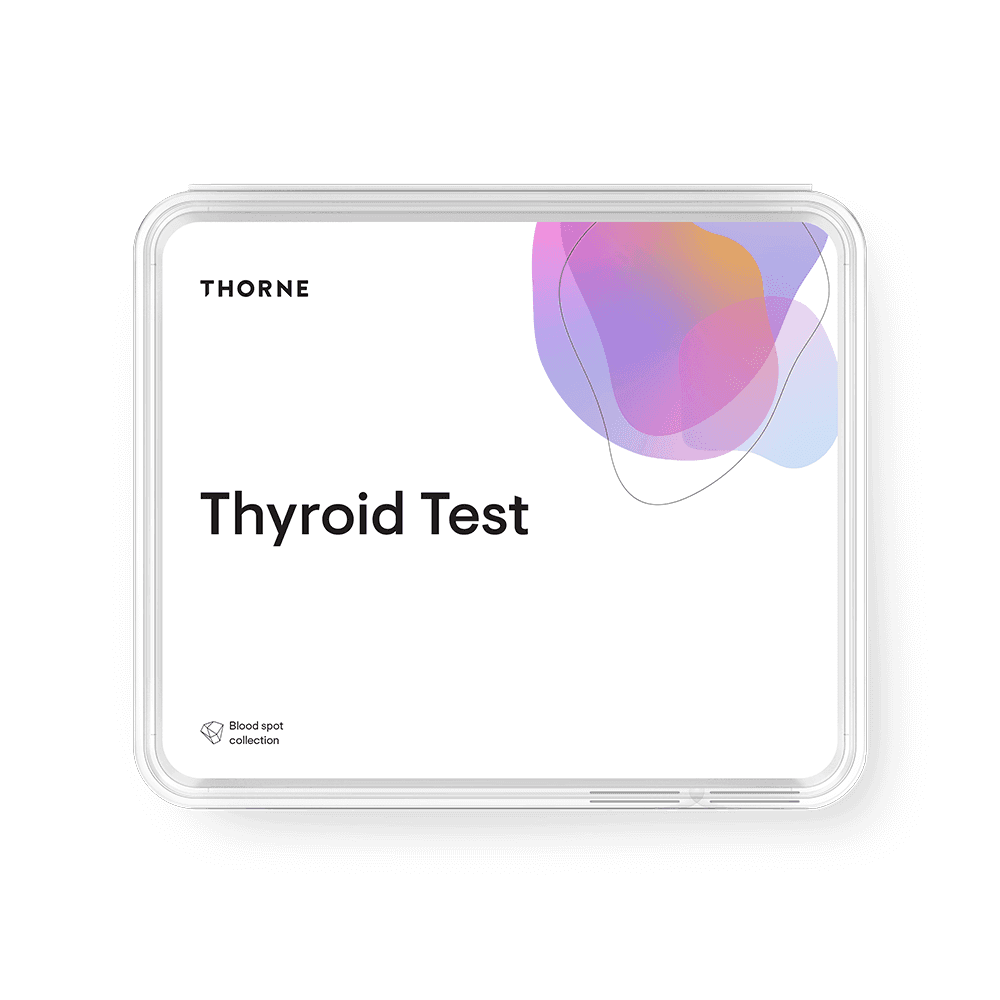
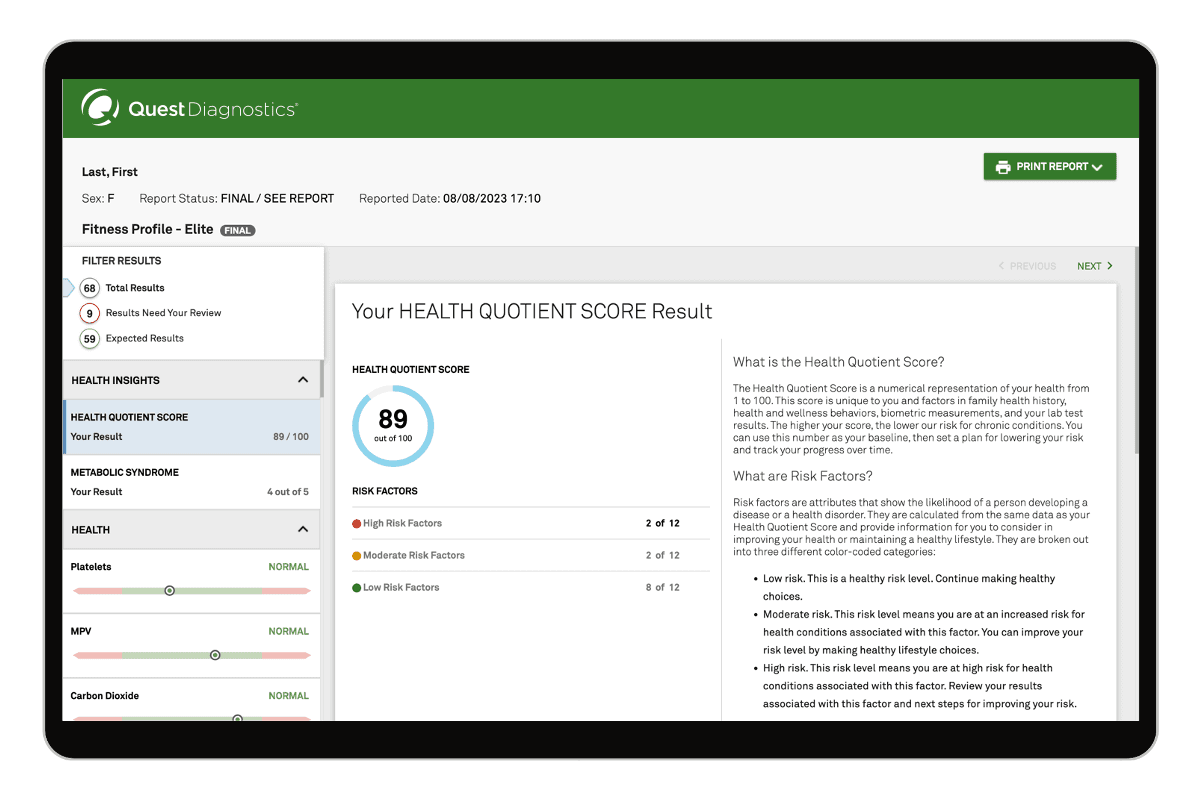
Diagnostics & Screenings
At age 40 with Hashimoto’s disease, the priority is tight thyroid control, cardiovascular and metabolic risk reduction, and early detection of related autoimmune and inflammatory conditions. This plan centers on routine blood pressure and lipid checks, diabetes screening, organ-function panels (CMP, CBC), targeted inflammation and autoimmune tests (hs-CRP, celiac screen), plus sleep apnea and skin cancer screening. Reassess annually and after any thyroid medication change. Plan ahead to begin colorectal cancer screening at age 45, and discuss prostate cancer screening in your 50s unless higher-risk factors arise earlier.
Screening Overview
| Tier | Test | Risk Area | Frequency | Why It Matters |
|---|---|---|---|---|
| Cardiovascular | Blood pressure measurement | Hypertension and cardiovascular disease | At every annual visit; check at home for 1–2 weeks if clinic readings are ≥130/80, then as advised by your clinician. | Hypertension affects nearly 1 in 2 U.S. adults; lowering systolic BP by ~10 mm Hg reduces major cardiovascular events by about 20%. |
| Cardiovascular | Comprehensive lipid panel (with optional ApoB) | Atherosclerotic cardiovascular disease | Every 5 years if low risk; every 1–3 years if you have autoimmune thyroid disease, family history, or prior abnormal results. | About 38% of U.S. adults have high LDL; elevated LDL/apoB drives plaque formation, and improving lipid levels cuts heart attack and stroke risk. |
| Metabolic | Hemoglobin A1c (A1C) | Prediabetes and type 2 diabetes | Every 3 years if normal; annually if BMI ≥25, family history, dyslipidemia, or elevated BP. | Roughly 1 in 3 U.S. adults has prediabetes and >80% are unaware; early detection and lifestyle change can cut diabetes risk by ~50%. |
| Organ Function | Comprehensive metabolic panel (CMP, including eGFR) | Liver, kidney, and electrolyte disorders; medication safety | Annually if you take long-term medications or have chronic conditions; otherwise every 1–2 years. | Chronic kidney disease affects ~15% of U.S. adults and is often silent; early detection slows decline and reduces cardiovascular events. |
| Organ Function/Hematology | Complete blood count (CBC) | Anemia, infection, and inflammation | Once a year, or sooner if you develop fatigue, pallor, frequent infections, or unusual bruising. | Iron or B12 deficiency anemia is common and can accompany autoimmune disease; anemia affects an estimated 5–10% of U.S. adults. |
| Thyroid/Autoimmune | Thyroid function tests (TSH with free T4) | Hypothyroidism control in Hashimoto’s disease | Every 6–12 months; also 6–8 weeks after any levothyroxine dose change or if symptoms change. | Optimizing thyroid levels reduces fatigue, weight gain, and lipid abnormalities; untreated hypothyroidism raises LDL and cardiovascular risk. |
| Inflammation/Cardiovascular | High-sensitivity C-reactive protein (hs-CRP) | Systemic inflammation and atherosclerotic risk | Get a baseline once; repeat every 6–12 months if elevated (>2 mg/L) or if your cardiovascular risk changes. | An hs-CRP above 2 mg/L roughly doubles cardiovascular event risk independent of LDL; inflammation is a modifiable contributor to CVD. |
| Autoimmune/Immunity | Celiac disease screening (tTG-IgA with total IgA) | Autoimmune enteropathy associated with Hashimoto’s | Once as a baseline; repeat if you develop gastrointestinal symptoms, iron deficiency, or have a strong family history. | People with autoimmune thyroid disease have a 3–5× higher risk of celiac; up to ~3–5% may be affected vs. ~1% in the general population. |
| Lifestyle/Risk | Obstructive sleep apnea (OSA) screening (STOP-BANG; home sleep test if positive) | Sleep-disordered breathing, hypertension, and cardiometabolic risk | Screen now; repeat every 2–3 years or sooner with weight gain, loud snoring, or daytime sleepiness. | OSA affects ~14% of men and increases hypertension, atrial fibrillation, and insulin resistance; treatment lowers BP and improves quality of life. |
| Cancer (Skin) | Full-body skin exam by a clinician | Skin cancer (basal cell, squamous cell, melanoma) | Every 1–2 years; sooner if you notice new or changing moles, have fair skin, or high sun exposure. | Skin cancer is the most common cancer; about 1 in 5 Americans develop it by age 70, and early melanoma detection yields >99% 5-year survival. |
Recommended Products
Nutrition & Dietary Focus
For a 40-year-old man with Hashimoto’s aiming to reduce inflammation and support immunity, prioritize a Mediterranean-style pattern, optimize selenium and vitamin D, use omega-3s, keep iodine adequate but not excessive (avoid kelp/iodine drops), cultivate gut diversity, consider a structured gluten approach, and time minerals away from any thyroid medication.
Recommendations
Anti-Inflammatory Diet Foundation
Adopt a Mediterranean-style plate: mostly plants (vegetables, fruits, legumes, whole grains), extra-virgin olive oil as the main fat, nuts/seeds daily, and limit ultra-processed foods and added sugars (aim <36 g/day). Target 30–38 g fiber/day.
Hashimoto’s—Selenium Optimization
Consider 100–200 mcg/day selenomethionine for 3–6 months with clinician oversight, or food sources (e.g., 1 Brazil nut most days; content varies). Keep total selenium <400 mcg/day.
Vitamin D for Immune Support
Check 25(OH)D and typically supplement 1,000–2,000 IU vitamin D3 daily with a meal; recheck in 8–12 weeks to maintain ~30–50 ng/mL.
Omega-3 Intake
Eat fatty fish (salmon, sardines, mackerel, trout) 2–3 times per week, or use a fish oil providing 1–2 g/day combined EPA+DHA if intake is low.
Iodine: Adequate, Not Excessive
Use iodized salt at home to meet needs (~150 mcg/day) but avoid kelp/seaweed supplements or iodine drops; keep seaweed foods occasional and in small portions.
Gut-Immune Axis
Include fermented foods daily (yogurt/kefir, sauerkraut, kimchi, miso) and prebiotic fibers (onion, garlic, leeks, asparagus, oats, beans). Consider a multi-strain probiotic if food intake is low.
Gluten/Celiac Strategy
Get screened for celiac disease. If negative but symptomatic, trial a gluten-light approach for 8–12 weeks (swap in oats, quinoa, brown rice) while meeting fiber, iron, and B vitamins; track symptoms and thyroid antibodies with your clinician.
Supplement Timing and Key Minerals
If taking levothyroxine, separate it from calcium/iron supplements, high-fiber supplements, and soy by 4 hours. Meet zinc (~11 mg/day) and iron needs via food (oysters, beef, legumes, pumpkin seeds); only supplement iron if labs confirm deficiency.
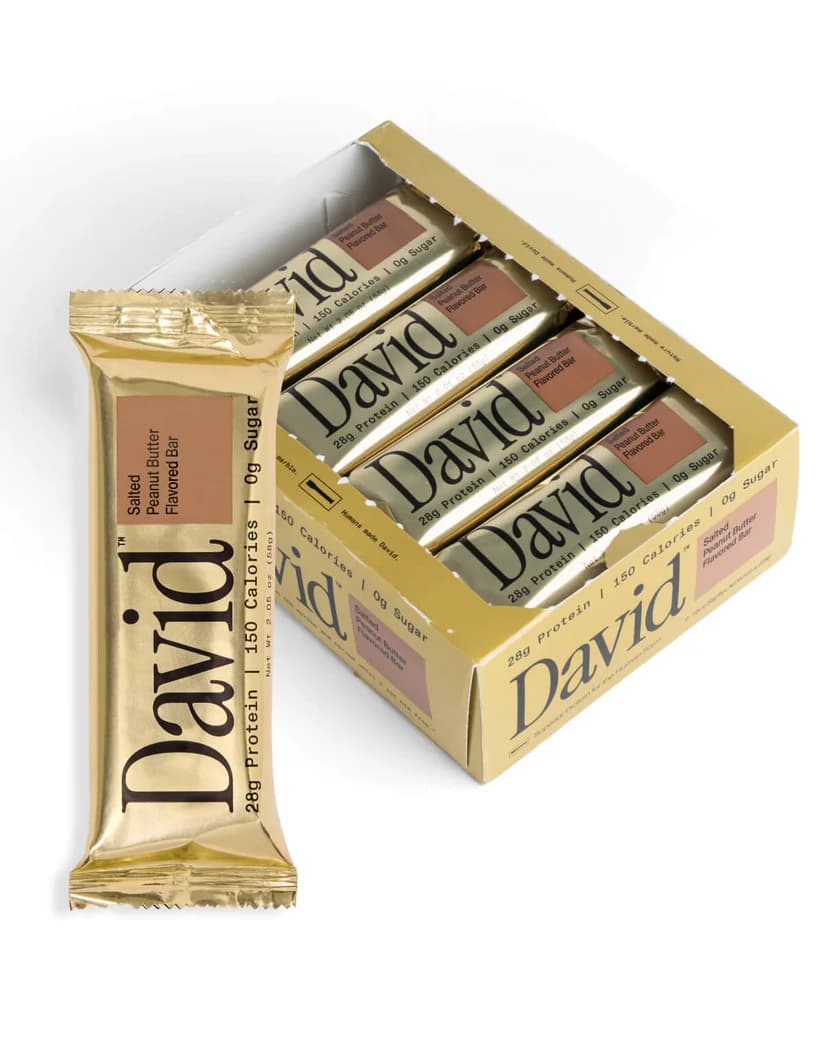
Recommended Products
Supplement Strategy
For a 40-year-old male with Hashimoto’s aiming to reduce inflammation and support immune balance, this stack focuses on nutrients that modulate thyroid autoimmunity, lower systemic inflammation, and maintain immune resilience. Emphasis is on selenium and myo‑inositol for thyroid antibodies, omega‑3s and curcumin for inflammation, and vitamin D, zinc, magnesium, and a probiotic for immune and gut support. Avoid high‑dose iodine and stimulating adaptogens (e.g., ashwagandha). Separate minerals from any thyroid medication by ~4 hours.
Supplement Recommendations
Selenium (as L-selenomethionine)
•Autoimmune/Thyroid100–200 mcg daily with food
Myo‑inositol
•Autoimmune/Thyroid600 mg twice daily (capsule or powder)
Vitamin D3
•Immune Support1,000–2,000 IU daily with a fat-containing meal
Omega‑3 Fish Oil (EPA+DHA)
•Inflammation Reduction1–2 g/day combined EPA+DHA (triglyceride form preferred) with meals
Zinc (as picolinate or citrate)
•Immune/Thyroid Support15–30 mg elemental zinc daily with food
Magnesium (glycinate or bisglycinate)
•Recovery, Sleep, and Immune Modulation200–400 mg in the evening
Curcumin (phytosomal/BCM‑95 or with piperine)
•Inflammation Reduction500–1,000 mg daily with meals
Multi‑strain Probiotic
•Gut–Immune Axis10–20 billion CFU daily (Lactobacillus/Bifidobacterium blend) with food
Recommended Products
Gut Health & Microbiome
For a 40-year-old male with Hashimoto’s focused on inflammation reduction and immune support, prioritize feeding microbial diversity (varied fibers and fermented foods), protecting the gut barrier (limit emulsifiers/alcohol; add soluble fibers and polyphenols), optimizing digestion and motility (meal hygiene and timing), and calming the gut–brain axis (sleep, stress, and vagal tone). Consider a careful gluten-light trial only if wheat worsens GI symptoms, and optionally a short probiotic trial to support barrier and immune balance.
Recommendations
Microbiome Diversity
Aim for 30 different plant foods per week and 30–38 g fiber/day. Include 5–10 g/day of prebiotic-rich foods (onion, garlic, leeks, asparagus, green bananas) and resistant starch from cooked–cooled potatoes, rice, or oats 3–5 times/week.
Fermented Foods
Include 1–2 daily servings of live-culture fermented foods (e.g., kefir, unsweetened yogurt with ‘live and active cultures,’ kimchi, sauerkraut, miso, tempeh). Rotate types and start with small portions if you’re gassy.
Gut Barrier & Inflammation
Limit ultra-processed foods with emulsifiers (e.g., polysorbate-80, carboxymethylcellulose) and excess alcohol; choose whole-food swaps. Add soluble, gel-forming fibers (oats, chia; optional 1 tsp psyllium) and polyphenol-rich foods (berries, extra-virgin olive oil, green tea).
Digestive Function
Practice ‘meal hygiene’: chew thoroughly, pause screens while eating, and finish the last meal 2–3 hours before bed. Take a 10-minute walk after meals. Before larger meals, consider a small portion of bitter greens or ginger (or a modest digestive bitters spray) if heavy meals cause bloating.
Gut–Brain Axis
Prioritize 7–8 hours of sleep, morning daylight exposure, and daily 5–10 minutes of vagal-toning (slow nasal breathing at 4–6 breaths/min, humming or gargling). Do brisk walking most days and 2 resistance sessions weekly.
Personalized Experiment & Targeted Support
If wheat/gluten seems to aggravate GI symptoms, try a structured 4-week gluten-light trial while keeping fiber diversity high, then reintroduce and observe changes. Optionally, trial a 12-week multi-strain Lactobacillus/Bifidobacterium probiotic (10–50B CFU/day), starting low. Take supplements at a different time than medications and confirm timing with your clinician. Consider a non-diagnostic stool microbiome test if you want a baseline to guide adjustments.
Recommended Products
Immune Support
For immune support with Hashimoto’s at age 40, focus on immune modulation—stabilize thyroid function, cover key micronutrients (vitamin D, selenium, zinc), follow an anti-inflammatory diet rich in omega-3s, stay current with vaccines, and prioritize sleep, stress control, and regular exercise. Avoid high‑iodine “immune” supplements that can aggravate autoimmune thyroiditis.
Recommendations
Thyroid stability and iodine caution
If prescribed levothyroxine, take it consistently on an empty stomach and separate calcium/iron/zinc by 4 hours; avoid iodine-containing “immune boosters” (e.g., kelp, nascent iodine). Keep regular TSH/FT4 checks with your clinician.
Vitamin D, selenium, and zinc status
Ask your clinician to check 25(OH)D; in NJ, consider D3 (about 1,000–2,000 IU/day) in fall–spring to maintain 30–50 ng/mL. Get selenium ~100 mcg/day (food or supplement; don’t exceed 200 mcg) and ensure zinc adequacy (food-first; short-term 15–30 mg/day only if needed).
Anti-inflammatory eating with omega-3s
Use a Mediterranean-style pattern: fish (salmon, sardines) 2–3×/week, plenty of colorful vegetables/fruit, legumes, nuts/olive oil; limit ultra-processed foods, added sugars, and excess alcohol. If considering gluten-free, screen for celiac first.
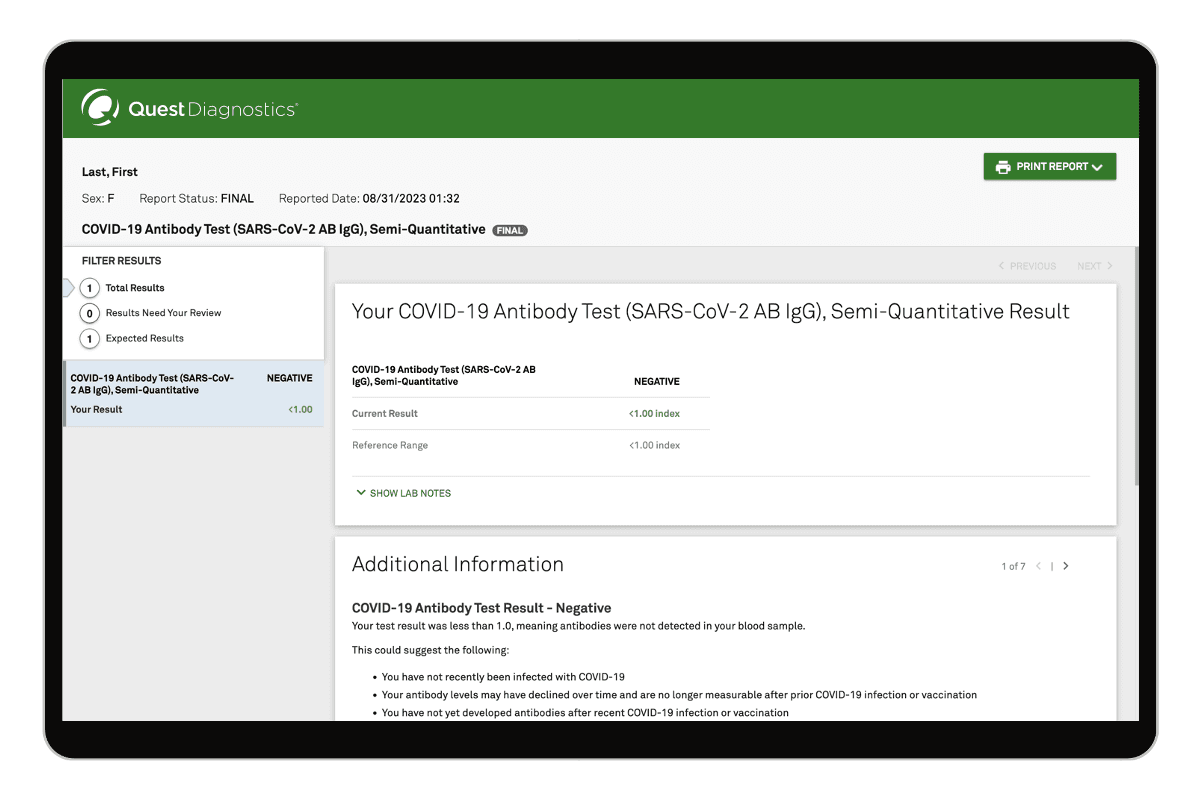
Vaccinations and infection prevention
Stay current with CDC-recommended vaccines (annual influenza; COVID-19 boosters as indicated). Practice hand hygiene and avoid close contact when ill outbreaks occur locally.
Sleep and stress regulation
Aim for 7–9 hours nightly with a consistent schedule, dark/cool room, and a 30–60 minute wind-down; add 10–15 minutes/day of breathwork or mindfulness and limit late-night screens/caffeine.
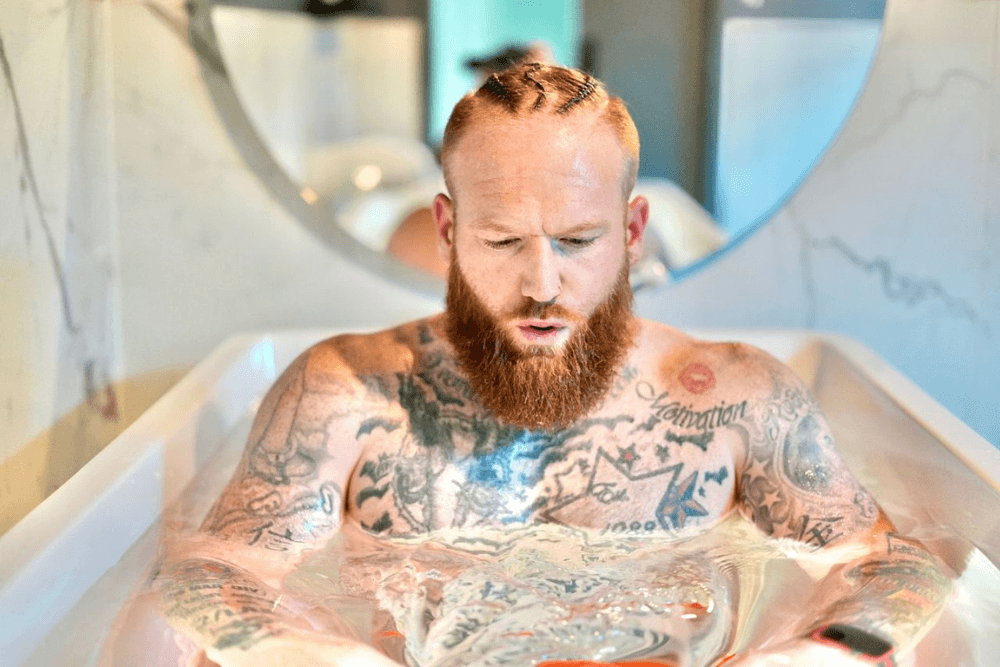
Regular activity and recovery
Target 150 minutes/week of moderate aerobic activity plus 2 days of strength training; include outdoor daylight exposure when possible and plan rest days to avoid overtraining.
Recommended Products
Inflammation Reduction
For a 40-year-old man in Hoboken with Hashimoto’s focused on inflammation reduction, prioritize a Mediterranean-style eating pattern, optimize omega-3s, manage thyroid-specific nutrients (selenium and iodine), ensure adequate vitamin D (especially through NJ winters), support gut health, and pair moderate training with quality sleep and stress control. Separate minerals/supplements from any thyroid medication by at least 4 hours.
Recommendations
Anti-inflammatory Eating (Hashimoto’s-friendly)
Base meals on vegetables (aim ~5 cups/day; include cooked crucifers like broccoli/cauliflower), legumes, berries, nuts, olive oil, and lean proteins. Limit ultra-processed foods, refined carbs, and added sugars (target <25 g/day). Keep alcohol ≤1 drink/day with 2+ alcohol-free days/week.
Omega-3 Optimization
Eat fatty fish (salmon, sardines, trout, mackerel) 2–3 times/week. If intake is low, consider a purified fish oil providing 1–2 g/day combined EPA+DHA with meals; choose low-mercury options.
Selenium–Iodine Balance (Thyroid-specific)
Get 100–200 mcg/day selenium (e.g., 1–2 Brazil nuts or a supplement if intake is low). Avoid high-iodine supplements/kelp; use iodized salt in moderation. Take minerals/supplements at least 4 hours apart from thyroid medication.
Vitamin D Status (seasonally important in NJ)
Ask your clinician for a 25(OH)D test; if low or borderline, supplement 1,000–2,000 IU vitamin D3 daily with a fat-containing meal and recheck in 8–12 weeks to personalize dosing (typical target 30–50 ng/mL per clinician guidance).
Gut Support for Immune Calm
Aim for 25–35 g/day fiber from diverse plants; include 1–2 servings/day of fermented foods (yogurt/kefir, sauerkraut, kimchi) if tolerated. If GI symptoms or persistent antibodies, consider a supervised 4–6 week gluten-light trial while maintaining nutrition; test for celiac before eliminating gluten if suspected.
Recovery, Sleep, and Smart Training
Accumulate 150 minutes/week moderate aerobic activity plus 2 days/week strength training; avoid daily all-out HIIT. Prioritize 7–9 hours/night sleep with a consistent wind-down and 10 minutes/day of breathing or meditation.